A Uniquely Male Concern: The Gut-Heart-Prostate Connection
Hello, I am Julie Donaldson and I am a clinical nutritionist with functional medicine training. I specialize in restoring balance in complex, chronic and acute health conditions. I welcome you to peruse other articles that may be of interest to you in your health investigation!
“Julie has helped me through a tough HPV and cervical dysplasia situation, and now she’s helping my husband through whole health and PSA problems. She is so educated and experienced on so many crossovers in health. Let yourself get started now!”
Emerging evidence is revealing important mediation by the gut microbiome of cardiovascular and prostate health in men. Poor gut health, systemic inflammation, hormonal imbalances, and lifestyle factors all increase the risk for both heart disease and prostate disorders. While heart disease and prostate disease do not directly cause one another, they share overlapping metabolic and inflammatory terrain. They are more commonly occurring together in the last number of years. Let’s break down the connections and what we have the power to do about them. Holistic health and proper testing are paramount, with a focus on determining root causes vs. symptom management.
It’s all about prevention in younger years, and the health of the gut is the center point of it all
While prostate cancer is most common in men over the age of 65, cases in men under 39 are increasing. (see below in The Role of Inflammation section for more information on this unfortunate trend) Steering clear of this very common cancer in men requires prevention and a mind for holistic connections. The gut is paramount.
It is well known that most diseases are 20 years in the making. Beginning healthy practices at age 20 prevents disease in mid-life in many cases. (Note also that digestive cancers are currently #2 in line behind prostate cancer at #1 in rates of occurrence.)
Unfortunately, many Americans have a lack of gut health with a balanced microbiome. Numerous pathogens can exist in the gut for long periods of time without creating noticeable symptoms. And while many might think this is a good thing, it isn’t. It’s stressful to have a blatant or raging gut infection, but at least we are flagged to do something about it when it happens.
When pathogens are at low levels and being “fought” on a chronic basis, the reserves of the immune system are being depleted. The body wants to heal itself…and it will keep trying, day in and day out, calling on all the warrior cells of the immune system. But if efforts fail to resolve an infection completely, eventually we have too much draining of the reservoirs. We also see destruction of the tight junctions of the intestinal walls (known also as leaky gut) I see this nearly every day in my practice.
While research is focusing on dysbiosis and its contribution to disease via inflammation, that research falls short on a couple of significant levels:
It isn’t focused on truly effective testing and protocol development
It isn’t focused on the individual and his unique genetic microbiome (there is no one-size-fits-all approach for every gut)
The intestine is the most significant interface between the internal body and the external environment. The maintenance of a stable intestinal barrier is crucial to prevent intestinal substances and pathogens from entering the internal environment. Intestinal homeostasis (which is the healthy and balanced state of the intestine) is determined by the intestinal epithelium, the gut microbiome, and the host immune system.
The gut barrier is a dynamic system influenced by the intestinal microbiome, and the activity of intercellular connections which are regulated by hormones, dietary components, inflammatory mediators, and the enteric nervous system (ENS). The ENS is also called the “second brain”, since it can regulate intestinal secretion and motility independently from the brain.
Leaky gut is mainly caused by bacterial infections, oxidative stress, alcohol or chronic allergen exposure, and dysbiosis, leads to the development of several pathologic conditions, including obesity, non-alcoholic fatty liver disease (NAFLD), non-alcoholic steatohepatitis (NASH), liver cirrhosis, neurodegeneration, cardiovascular diseases, inflammatory bowel disease, celiac disease, irritable bowel syndrome, type 2 diabetes, and several autoimmune conditions.
The direct connection between compromised gut/immune health, metabolic disease and cardiovascular disease is documented here. Men develop heart disease at twice the rate women do.
The direct connection between compromised gut/immune health, metabolic disease and prostate disease is documented here. Current statistics are that 1 in 8 men will develop prostate cancer.
The role of inflammation
Once again, the focus needs to be on “non”-inflammatory vs. anti-inflammatory. The latter is prevalent in our society - we love to discuss what can de-inflame. But once we’ve hit the point of inflammation, the job is much harder and more complicated. Here at True Nature, we talk constantly about PREPARE-PREVENT-PREVAIL.
In this scenario, Prepare-Prevent-Prevail means achieving a balance of healthy bacteria, short chain fatty acids (SCFAs), bile acids and action upon the endocannabinoid system. All of these factors in a biochemically, individual balance create a symbiotic relationship with the immune system, especially the maturation of the innate immune system which protects us against inflammation and disease.
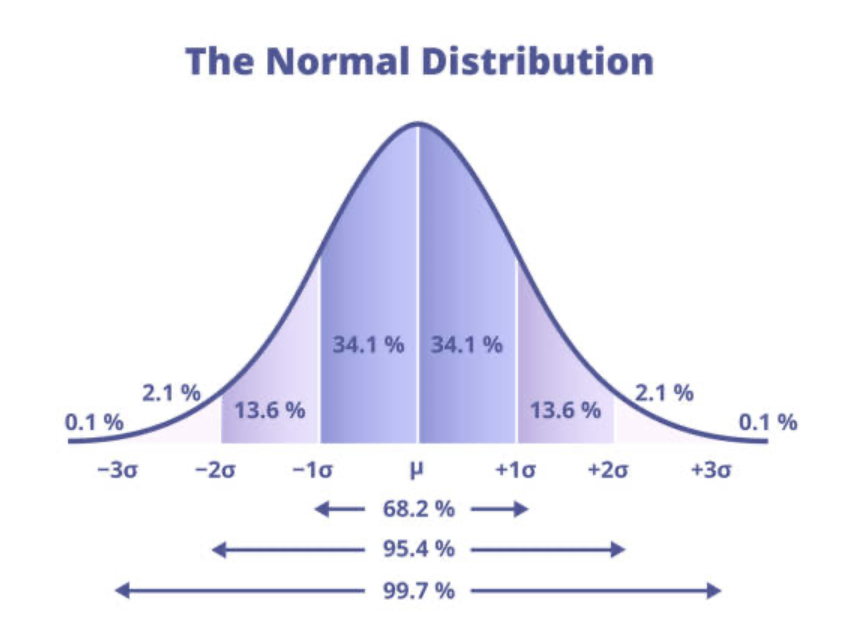
Bell curve distribution
If inflammation occurs as a result of infection- namely the stimulus of the Bell curve of inflammation (which may remain at the top and fail to resolve back to normal) - we ultimately get disease. This often occurs when inflammation is repetitive, chronic and/or severe.
Diseases that are associated with unresolved inflammation include diabetes, IBS, cardiovascular disease and liver-related diseases (including NAFLD). Remember, we have connected the gut with cardiovascular disease and prostate cancer here. The latter can also be connected with diminished liver function and/or disease. In particular, failure of the liver to produce CYP enzymes which clear toxins such as petroleum-based, plastics & estrogen-rich compounds. This is one of the reasons for the rise in younger male cases of prostate cancer, as we are exposed to more and more of these toxic compounds. Also a contributing factor is the rise in use of toxic chemicals in farming practices.
Summations and Solutions
We all know the statistics of how common heart disease and prostate cancer are for men. But it’s only recently that they are connected to one another as well as to gut health. Inflammation is the connection. And waiting to try to alter the big patterns of inflammation after they’ve set up is much harder than creating a non-inflammatory scenario. This takes preparation and some baseline testing to establish.
These are the key pieces:
Identify & make a lifestyle of your personalized MT nutrition (this also helps to stabilize your genetic microbiome)
In addition to personalized nutrition, always eat clean, fresh, sustainable food, avoiding preservatives and sugar.
Utilize a personalized protocol with pre and probiotics as well as SCFAs.
Test your blood with PSA included
Test your gut
Monitor periodically following protocol use
Please email me at Julie@truenaturehealthconsulting.com for more information. We provide telehealth services.