ADHD on the Rise: Dopamine, Immunity, Brain Fog and Solutions
Hello, I am Julie Donaldson and I am a clinical nutritionist with functional health training. I specialize in restoring balance in complex, chronic and acute health conditions. I welcome you to peruse other articles that may be of interest to you in your health investigation!
“Having dealt for several years with our child’s ADD challenges, it wasn’t until Julie helped us that healing really happened. We got lots of advice from all the typical sources and it all helped in little bits. But with her approach we got profound change, and our son no longer has school or behavior problems. Also, our own fears of addictive problems coming into play have disappeared. We trust her implicitly.”
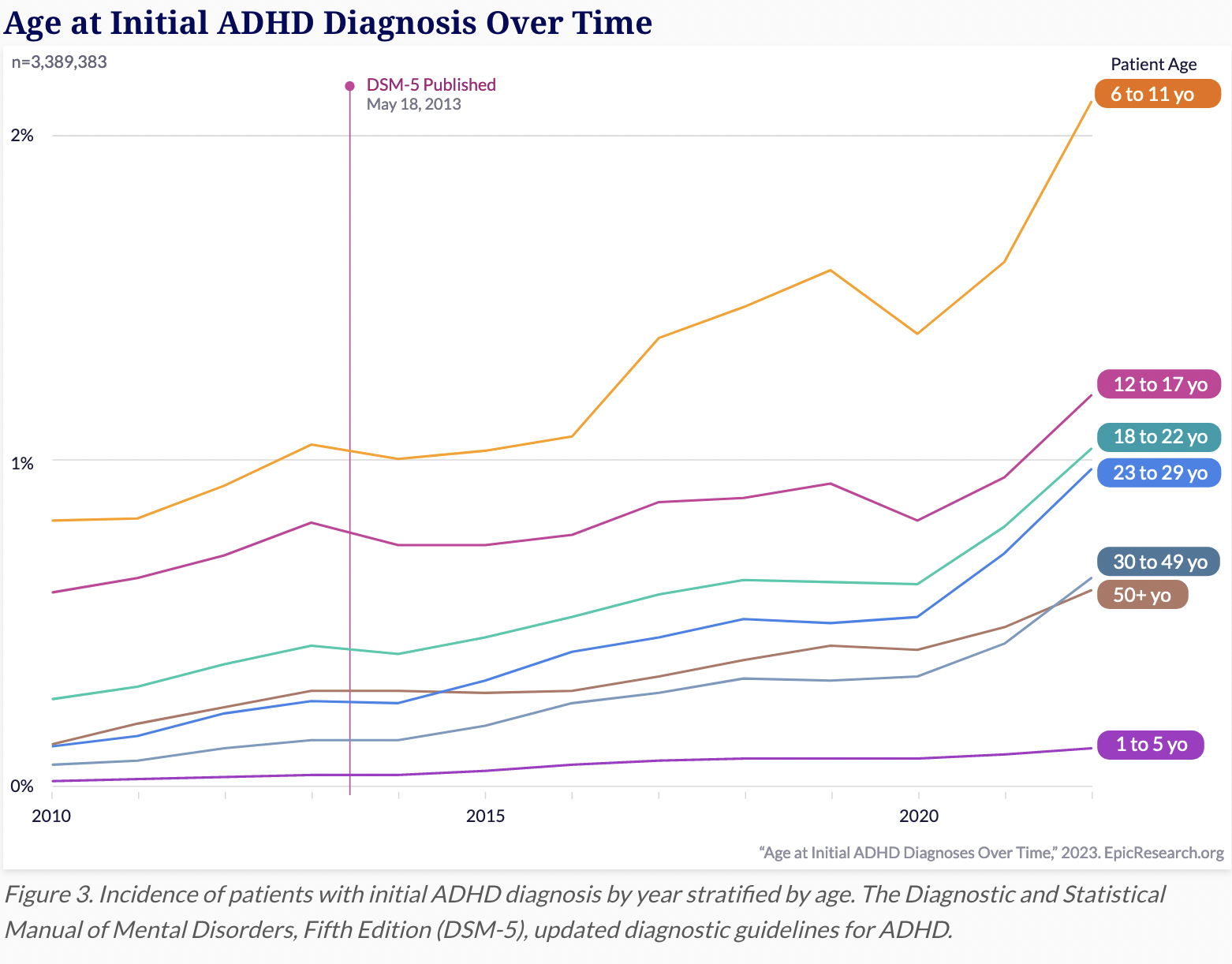
For many years, the rise in diagnoses of ADHD (Attention Deficit Hyperactive Disorder) has been attributed to better awareness and familial patterning. While this may be an important factor in diagnosis, most certainly we need to be looking more carefully at the inflammatory and immune relationships with ADHD and ADD. Virtually the entire world population has been exposed to a significant virus and/or to a significant vaccine that has the potential to increase cytokine activity in the body. From 2020-2022, the rate of diagnosis for females aged 30-49 literally doubled. All age groups had considerable increases in diagnoses during these two years, unlike the slower, steady increases observed over the last decade. Additionally, for many adults who suffer from brain fog - this may actually be “adult ADHD”. Let’s talk about inflammation, immunity, dopamine, brain fog and attention deficit intersections.
ADHD diagnosis rates by age
What are attention deficit disorders?
Both ADHD and ADD are much more commonly diagnosed in children and young teens than in adults. This is primarily due to the hyperactivity concerns that are prevalent in children. As people age with ADHD, hyperactivity decreases - yet the feeling of being “wired” and unable to shut off the brain remains. Also, as people with ADHD age, whether diagnosed or not, hyperactive behaviors decrease but addictive and self-medicating tendencies increase. (More on this topic later in the article.)
Attention deficit disorders are characterized by the following behaviors and symptoms:
inability to pay attention/focus on tasks or hyper-focus
boredom
need to be active and/or talkative
poor memory
impulsivity
fatigue, daytime drowsiness, insomnia*
inability to calm the mind and thoughts, easily distracted
dyslexia and dyscalculia
Many of these problems can feed one another. Poor sleep, for instance, feeds poor attention/focus and fatigue.
Approximately 50% of those with ADHD suffer from some degree of insomnia. Any combination of factors can produce a self-perpetuating loop through the symptomatic spectrum. (Dopamine and norepinephrine play significant roles in the balances of serotonin and GABA, both critical for initiating and maintaining sleep throughout the night. Dopamine is discussed in greater detail below.)
Children who suffer these conditions are often red-flagged in school and their siblings are now more likely to be assessed and diagnosed due to recognition of the pattern running in families. A number of longitudinal studies suggest that up to 60% of children with ADHD go on to have significant behavioral and psychiatric problems in adolescence and adulthood. When compared with children without the disorder, ADHD children have lower education, lower income and higher unemployment over time. Criminality and substance abuse rates are also higher. Between 50 and 80% of ADHD patients have comorbid psychiatric disorders including anxiety, depression and conduct (impulse control) disorders. They are more prone to accidents, divorce, financial issues and work conflicts. Given all of this and the reality of the disorder continuing into adulthood, it is paramount to understand how to identify and effectively support the individual to heal from ADHD.
Let’s talk about some common root causes, some of which can be genetic and many of which can be environmental.
First, let’s discuss food. It is well accepted in the ADHD/ADD communities that poor nutrition is a major risk factor. The brain uses 20-25% of the total metabolic requirements in the body. Even mild nutrient deficiencies will affect function.
While we get a lot of our nutrients from food, we also need to consider that there are certain vitamins and minerals that may need to be supplemented. The association of ADHD with MTHFR mutations has been made clear. Specifically, those with the 1298A>C polymorphism have a higher incidence of ADHD. This requires special attention to methylation expressions (observed in blood testing) and application of B vitamins, zinc, selenium, magnesium, etc.
There is a multitude of research showing that food sensitivities, additives, dyes and low protein are common causes of ADHD. A whole food diet with low sugar, adequate protein and no preservatives or additives is necessary to remove this influence. In this study, it was shown that healthy diets lowered the risk for ADHD by 37%, whereas junk food diets significantly raised the risk for ADHD development.
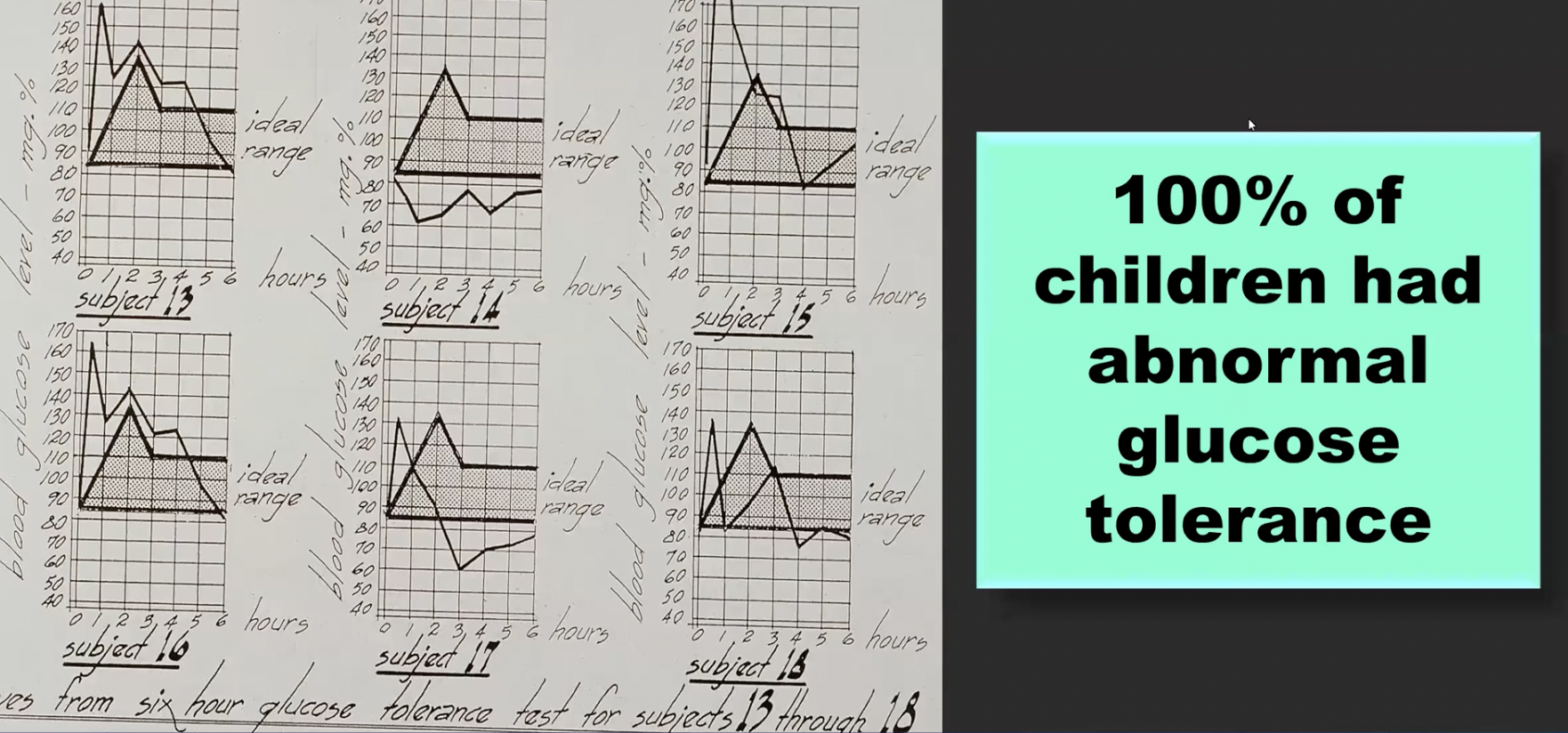
Over 20 years ago, Shirley Lacy, PhD compiled studies on children with ADHD and found 100% of study participants had abnormal glucose tolerance. Below are photos of her documented graphs.
ADHD subjects and abnormal glucose tolerance, Dr. Shirley Lacy
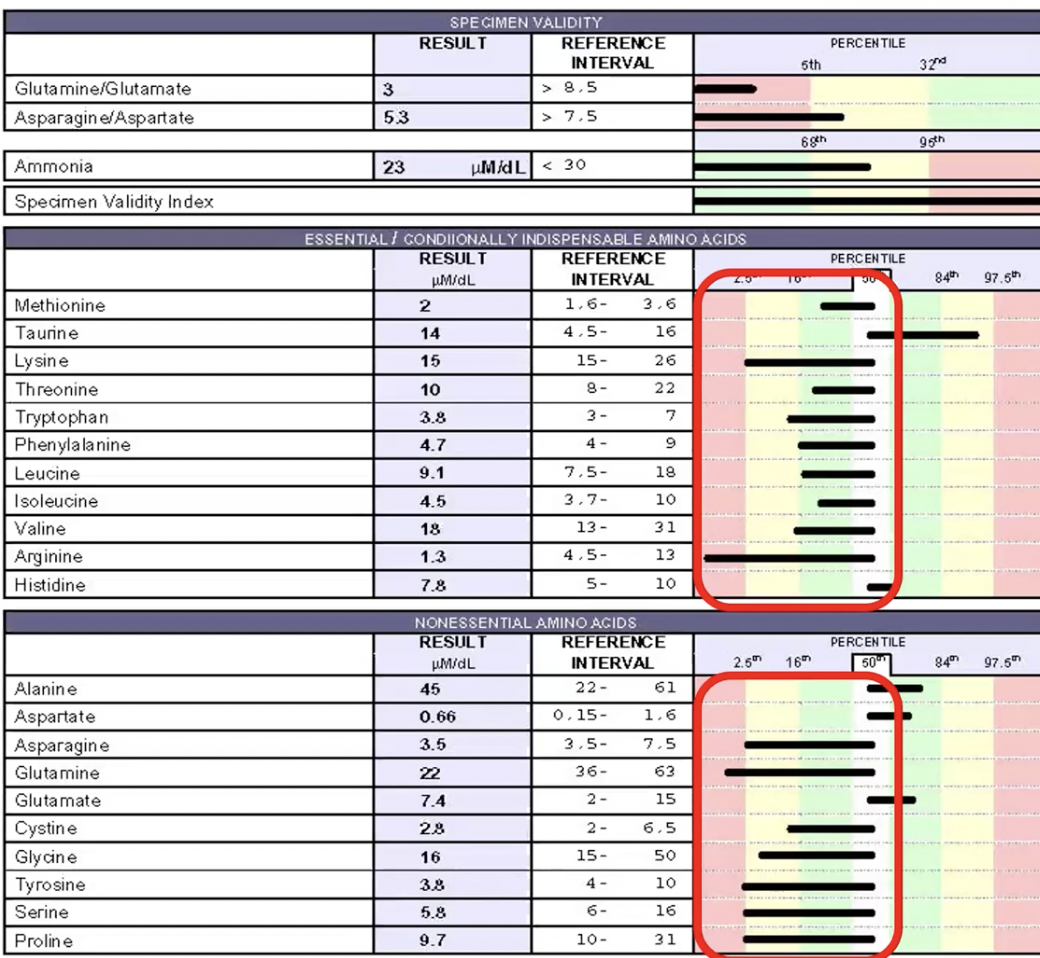
As it relates to amino acids (proteins) and ADHD expression, many of those with the disorder have low levels of certain amino acids:
ADHD children and amino acid deficits
Amino acids are absolutely critical for a multitude of functions in the body. Those with low amino acid intake or gut stress that impedes proper digestion will suffer from impaired function, inclusive of mood and executive regulation, detoxification and cellular building and recycling. In addition to amino acids we also require essential nutrients such as fats, vitamins and minerals that our bodies cannot make on their own. Whether missing from the diet or poorly digested due to gut dysbiosis, these are key elements for healing from ADHD.
Amino acid functions and digestion
Note: many people have heard of neurotransmitters but not of neuropeptides. A neuropeptide can modulate (increase or decrease) a postsynaptic response in the brain to a neurotransmitter. In this capacity, neuropeptides influence many of the prior-mentioned functions, including reward, food intake, metabolism, reproduction, social behaviors, learning and memory.
Below are the results of a urine amino acids test taken by a person with ADHD:
Low amino acids test result
Toxins, especially heavy metals are a culprit. Dr. James Greenblatt, an expert in ADHD and neurotransmission states that the following things must be removed for healing to occur with ADHD:
Copper
Lead
Pesticides
Sugar
Phosphates
Artificial sweeteners
Gut dysbiosis
Brainwave imbalances (please note that neurofeedback practices are well researched to support this aspect of
ADHD)
Lead toxicity has been clearly associated with the expression of ADHD. (Note that children can be exposed to lead in utero.)
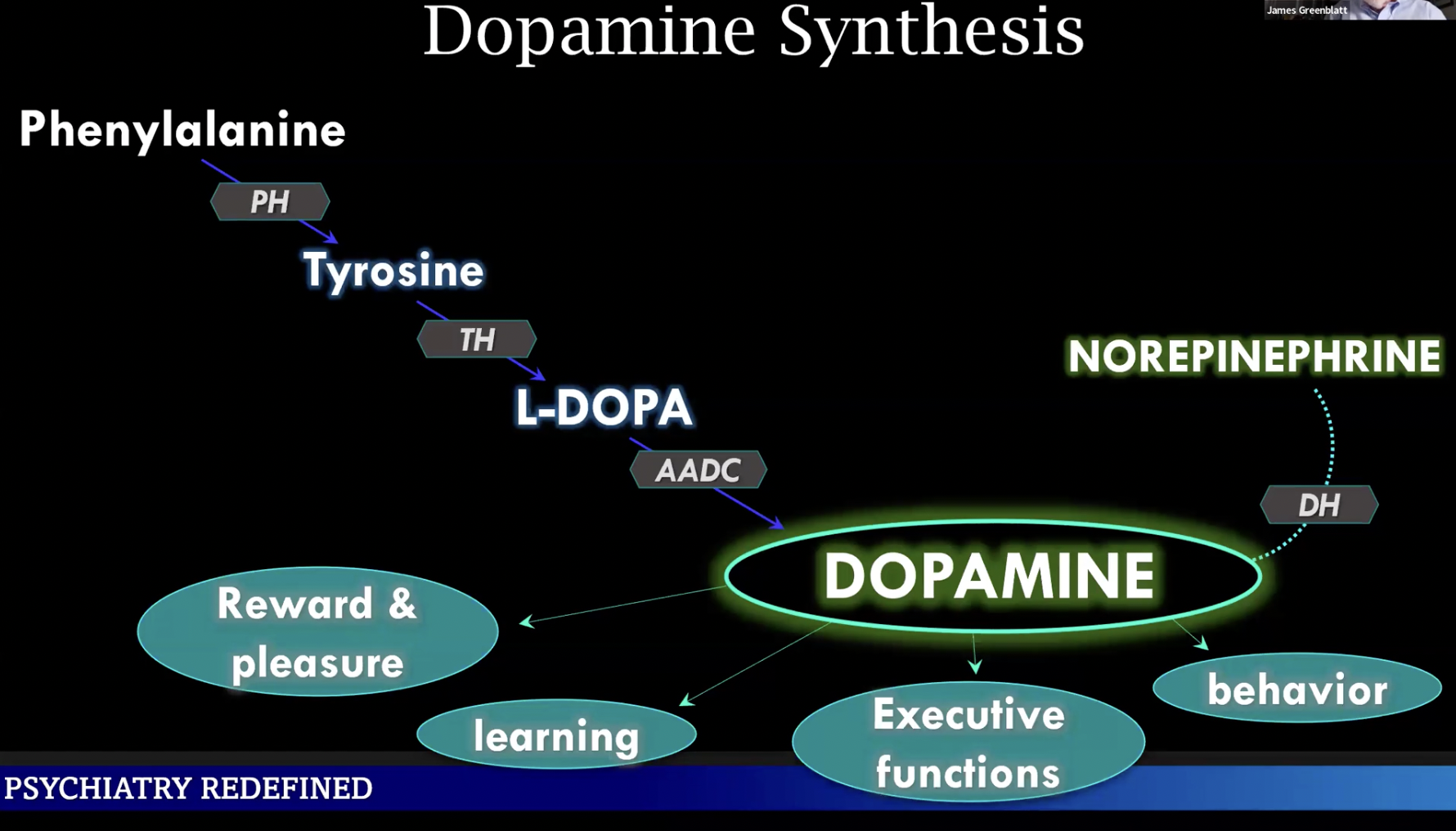
Also very clear is the role that low dopamine plays in the development of ADHD. Dopamine is a neurotransmitter that regulates emotion, motor control, motivation, cognition and vascular function. Dopamine is a chemical messenger in the brain known as the “reward chemical” - it is responsible for the pleasure/reward system in the brain. It is also called a “motivation molecule”, as it provides the focus and drive we need to be productive.
There are 5 dopamine receptors in the central nervous system and brain, all associated with genetic predisposition (DRD1-5). As we know from all of our conversations, while genetic polymorphisms need to be taken into consideration, epigenetic lifestyle influences can help to turn off these genetic switches, allowing normalized function. Toxic substances may affect the dopamine system in early development and contribute substantially to the etiology of ADHD . Additionally, in response to stress, fetal adaptations in dopamine systems may alter early development with lasting effects. Thus, it is not only the health of the child but the health of the conceiving parents that is of great impact in turning off these switches.
Vitamin D is key to adequate dopamine production. We speak a good bit about how to maintain D levels here at True Nature. Of utmost importance are 2 major things - 1) we need adequate vitamin D supplementation, along with vitamin K and 2) we need to have balance in the redox system between helpful oxidants and antioxidants that allows the Vitamin D Receptors (VDRs) to function normally. With an abundance of free radicals & ROS (Reactive Oxygen Species) in the body, a byproduct of lipid peroxidation is found in those with ADHD, and that is ethane. Individuals with ADHD often have an excess of ethane in their exhaled breath. This is a gaseous compound that is toxic to the body. In lipid peroxidation, ROS break down healthy omega 3 fatty acids which oxidize and produce this gas. These same ROS also damage dopamine-producing cells and cause dopamine oxidation. Children with ADHD have low Total Antioxidant Status, as per the research.
Oxidative stress in the brain, in particular, can harm neurons. And it is known that ADHD medications increase oxidative stress and decrease glutathione in the body.
High extracellular dopamine and low reception at sites in the brain are consistently found in those with ADHD. Note from the chart below that above-mentioned low amino acids (tyrosine & phenylalanine) are precursors for dopamine. When low, functions associated with regulated dopamine will be impaired. These impairments may predispose a person to addictive behaviors.
Dopamine synthesis
Addiction is an (unfortunate) common outcropping of ADHD. In his book “Life with ADHD”, Peter Jaska PhD states that 50% of those with ADHD/ADD develop addictions. It is also known that 25% of addicts are diagnosed with ADHD. In a Harvard Medical School study of young adults with drug or alcohol use, Dr. Timothy Williams found that only 30% are using substances to “get high”. The other 70% are self-medicating for tension, sleeplessness, etc. This points to a high percentage of users attempting to calm a heightened nervous system rather than “using” for the experience of a high.
Addiction also involves imbalances in dopamine and the dopaminergic system. When dopamine is low, drugs and non-substance (shopping, pornography, work, gaming) addictive behaviors provide temporary “lifts” in the system. The challenge, of course, is that this experience is addictive and over time, more and more of the drug or behavior is required to produce the same amount of dopamine.
Brain fog - the “kissin’ cousin” to ADHD
Brain fog is a more common complaint amongst adults than ADHD - for many experts in the field, it is actually considered to be “adult ADHD”. While young people may experience brain fog as well, the hyperactivity that is associated with youthful ADHD tends to override those symptoms.
So, what characterizes brain fog?
mental fatigue
forgetfulness
an inability to pay attention (not caused by distraction)
slow physical movement
difficulty finding words
incoherent or jumbled thoughts
careless, random mistakes
drowsiness, feeling sedated
When potentially a form of “adult ADHD”, brain fog can also include the feeling of being “wired”, even though not focused nor moving quickly. Mental activity can include obsessive thoughts and be very persistent - again - in spite of slow mental processing. It is estimated that 54% of those diagnosed with ADHD also have brain fog, sometimes referred to as CDD, or Concentration Deficit Disorder.
Brain fog has been described by experts as the subjective experience of neuroinflammation - a fancy word for inflammation in the brain/nervous system caused by toxic and immune stresses. I have written about the neuroimmune loop, which you can read about here - we’re essentially describing the same thing. There is significant research on the immune component of ADHD. Let’s take a look.
How do cytokines and immune inflammation come into play with ADHD?
Research has shown: 1) people with ADHD have higher cytokine levels than control groups without the condition and 2) chronic immune inflammation is associated with ADHD.
Cytokines are a broad group of signalling proteins that are produced after cellular activation and act as body fluid antibody regulators. They modulate the functions of individual cells and regulate processes taking place under normal, developmental and pathological conditions. When cytokine activity remains chronically high, the immune system is not returning to homeostasis, but rather remaining in an inflammatory state. Because cytokines involve antibodies, the risks for autoimmune-type responses are high with lingering elevations.
So, what else is impacted with chronic immune inflammation? Converging evidence suggests that the mesolimbic dopamine (DA) system is directly affected by increases in inflammatory cytokines associated with chronic, low-grade inflammation. This information helps us to understand that while ADHD is highly heritable, it can also be a condition that develops later in life based upon negative epigenetic influences - namely, immune stress.
While any significant immune condition can trigger this response, here we specifically address the research identifying cytokine elevations associated with COVID-19. With this, I point back to the statistics mentioned in the very beginning of the article that relate to dramatically increased levels of ADHD diagnosis in the last two years.
In this study of hundred of COVID survivors, a high frequency of cognitive impairment was found, inclusive of executive functioning, mental processing speed, fluency, memory and recall. Also studied with COVID are the elevated levels of cytokines, including interleukin-6, interleukin-1, interleukin-17 and tumor necrosis factor-alpha.
Summations and solutions
The brain and nervous system power the entire body. Imbalances in neurotransmission and/or neuroimmune activity can cause daily, grinding stress on any person of any age. Let’s talk about how to prevent this condition from being a lifelong stress.
Brain power
As is always the case, conventional medication for attention deficit disorders has side effects and risks for other serious responses. In functional health care, we are always focused on what the root causes are and how to correct them naturally - fortunately, there are options.
Here are a number of key factors that must be considered and investigated when dealing with ADHD:
Define and implement personalized nutrition, including the application of Metabolic Typing® and only clean, whole foods. Remove all foods containing preservatives, dyes, chemicals and pesticides.
Define and implement targeted appropriate testing for the biochemical evidence of ADHD. This may include blood chemistry, hair analysis for heavy metal evaluation, amino acids testing and Dutch hormone testing. This combination of tests identifies all of the risk factors and provides a baseline for the measurement of therapeutic success. In response to test results, in the hands of a skilled practitioner (please do not self-diagnose or treat), a number of natural substances can be utilized to correct imbalances and restore well-being. These include, but are not limited to glutathione, DLPA, SAMe, vitamin B6, zinc , vitamin D and lithium. We may also need to consider specific substances that encourage dopamine to remain around the synapses in the brain for longer period.
Develop regular exercise habits. Research shows improvements in confidence, motor skills and executive functions in those with ADHD/ADD.
Practice daily breathing exercise. Research also shows that controlled diaphragmatic breathing improves cognition, affect, attention and cortisol levels. See the video below for 4 controlled breathing techniques that have also been shown to create 24-hour positive effects on the nervous system.
Investigate air quality in all environments regularly visited and implement filtering as needed. Air pollution is also associated with brain fog - this includes outdoor pollutants as well as VOCs (volatile organic compounds) from indoor construction and textiles.
Connect with educational resource agencies for the latest information on ADHD-specific support. Here are two excellent sources for professional information:: https://chadd.org/research/; https://www.addrc.org/why-adhd-is-on-the-rise/
Please contact me at Julie@truenaturehealthconsulting.com for personalized support and evaluation. We provide holistic telehealth services which are developed for the individual.