Bone Loss, Elevated Homocysteine, Individualized Nutrition and Cardiovascular Disease: Exploring New Testing and Functional Support
Hello, I am Julie Donaldson and I am a clinical nutritionist with functional medicine training. I specialize in restoring balance in complex, chronic and acute health conditions. I welcome you to peruse other articles that may be of interest to you in your health investigation!
“I was one of those people prescribed medication and excess calcium for bone loss. I watched my scores worsen over the years instead of improve. Julie is the one who put all the puzzle pieces together for me and now I am healing. Do NOT wait to talk with her! Every day counts,
and she knows the intersections of these issues like no one I have ever met before.”
Osteopenia (bone softening) and osteoporosis (bone loss with fracture risk) are the two types of poor bone density conditions. Many people think bone loss only affects the elderly. Many people also think bone loss is an isolated problem unto itself and that it is strictly a female problem. This article will shed important light on the intersections between homocysteine, bone loss, individualized nutrition and increased mortality rates, primarily in the category of cardiovascular disease, as well as the truth about men and bone loss. As our world becomes more toxic and the mass media one-size-fits-all approaches to nutrition increase, more people will be at risk for poor bone remodeling and increased mortality rates. New information on microplastics and bone loss will also be discussed here.
Let’s take a look at the multitude of factors that influence these functions and how they are intersecting with one another. We’ll also look into wonderful new technologies and nutrients that are adding to a more comprehensive and holistic view of bone health.
What makes bone strong?
How is bone remodeled? mineralization and resorption…
Throughout life, cells in the bones known as osteoblasts construct the bone matrix and fill it with calcium. At the same time, osteoclasts in the bones work just as busily to tear down and resorb bone. This fine balance is regulated by many factors, including systemic hormones and immune cytokines. Cofactors such as vitamin D, zinc, magnesium, silica, phosphorus and boron are all needed to balance the calcium driven into the bones and/or resorbed. Thyroid and parathyroid health must also be considered in this mix.
Occurring simultaneously with bone formation and resorption is collagen cross-linking.
Collagen is an essential part of the framework of the design of our various body tissues. It is the major insoluble fibrous protein in the extracellular matrix and in connective tissue. The extracellular matrix is key for cell differentiation, stem cell differentiation, bone remodeling and wound repair.
It is the single most abundant protein in the animal kingdom. Collagen makes up 25% to 35% of the whole-body protein content. It consists of amino acids (proteins) bound together to form a triple helix of elongated fiber known as the collagen helix. This creates a structural role in the body.
It is present in large quantities in connective tissue and provides bone, tendons and ligaments with tensile strength and skin with elasticity. It often works in conjuction with other important proteins such as keratin and elastin.
Collagen production declines with age and exposure to factors such as smoking and UV light.
There is a process called collagen cross-linking which is operating in bone mineralization as well. Through the bonding of proteins, collagen utilizes cross-linking to promote a change in the physical property of the bone. We will cover more on this topic below, as well as more on the tensile strength of bone.
Bone mass reaches its peak by the middle of the third decade of life and plateaus for about ten years, during which time bone turnover is constant, with bone formation approximately equaling bone resorption. While bone loss is often described as an “age-related” problem, here at True Nature, I view most of these problems as layered, long-term stresses that involve deficiencies, toxins and improper nutrition for the individual’s needs. Osteoclasts can gain the upper hand in decreasing bone mass over the years and certainly hormone levels can play a role in this. We should not, however, leave out a multitude of other factors that could be optimized for much longer than the standard 50 years before bone loss typically begins. Conversely, the more complicating and layered factors a person is burdened with, the more exponential the bone loss can be.
What about men vs. women and bone loss?
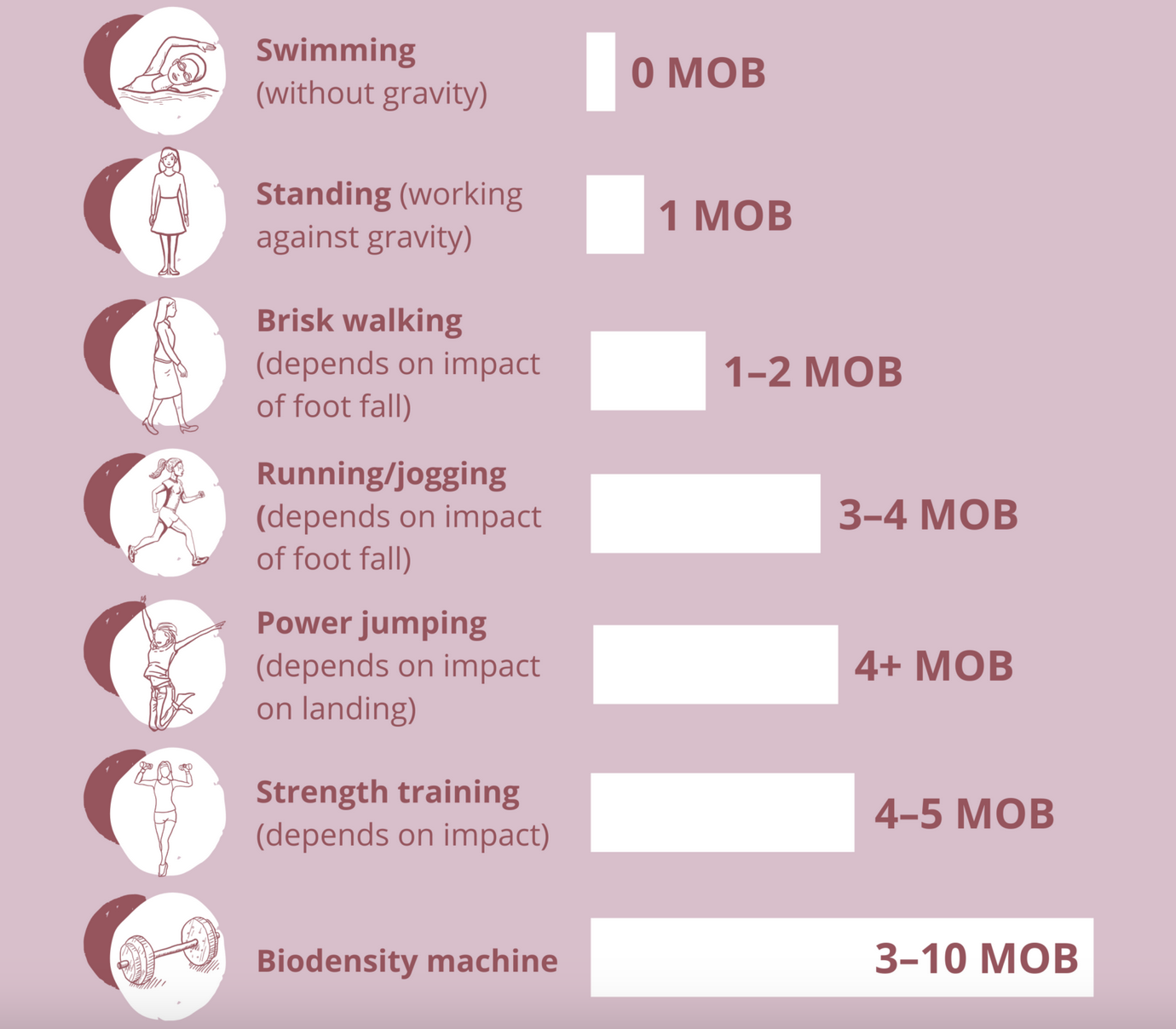
While the major focus is on women and bone integrity, men are also susceptible to bone loss. Oddly enough, in earlier years, men have a higher rate of osteopenia (softening of bone without fracture) than women. In this study, younger men were found to have a 28% rate of osteopenia while women had a 26% rate. While there needs to be much more research on men and bone loss, we may be able to decipher a few possible risk factors for this surprising fact. Note that the men in the study preferred cardio exercise to weight-bearing exercise - another surprising finding. Weight-bearing exercise has been touted to help maintain bone strength and mass. It has been researched, however, that the lower body requires 4.2 times its own weight to stimulate new bone growth, while the upper body and core require 1.5 and 2.5 times the body’s weight.
Multiples of body weight (MOB) by activity, image credit Better Bones
Research reports that the following extracellular diseases/conditions impact men more than women:
alcoholism (defined as either daily intake, or greater than 10 servings per week)
low BMI
glucocorticoid excess
hypogonadism (low sex gland function)
hyperparathyroidism
gastrointestinal disorders (malabsorption, IBD, gluten intolerance)
biliary cirrhosis
neuromuscular disorders
cardiovascular events
Another potential factor is diet and supplementation. In general, women tend to monitor these things more closely than men, who have lower overall interactions with their health care. Diet has also been posited as a cause for this problem, as women also tend to be more involved in nutritional and supplement programs than men do. Low nutrient diets and inadequate mineral intake are real concerns with bone integrity.
Let’s talk about a couple of other fascinating findings on men and bone loss. First, scientific evidence shows that men have more osteoporosis-related complications and a higher mortality rate after osteoporosis fractures than women.
Second, fragility fractures are correlated with another measurement of bone integrity called the Trabecular Bone Score (TBS). Evidence shows, interestingly, that men with osteoporosis who undergo fragility fractures have greater loss of trabecular connectivity than men with osteoporosis without fractures. We will cover TBS in more detail below. It is a new and impactful addition to the conversation about testing and tracking bone integrity.
Individualized nutrition and bone integrity
At True Nature, we practice individualized nutrition. It is the foundation of all healing and of the body’s ability to repair itself from disease and damage. As discussed in this important article, our ability to produce ATP (the energy to all of our cells), we must give the Krebs cycle the balance of nutrients it requires for how our individual body is metabolizing. This allows for mitochondrial respiration, which produces ATP. If you eat what I eat and we have a difference in how we process our nutrients and thus an alteration in the successful completion of our Krebs cycles, one of us may do well and the other may suffer. When energy is not optimized in nutrition, the body has to prioritize which functions it will complete. This means setting aside other important repairs, immune responses, detox, etc, due to a lack of ATP/energy. The body can only respond to demand with the available amount.
These metabolic differences in individuals also includes what minerals are most required to help speed up or slow down metabolic processes. One person may need a higher amount of calcium, another may need a higher amount of magnesium, zinc or phosphorus. Metabolic Typing®, which is the format of nutrition used in this practice, allows for and prescribes foods and supplementation for those differences. If a person is eating in a manner that is contrary to those needs, the issue of bone remodeling can absolutely arise.
As all of us know, the discussion of bones and bone loss is treated in the medical world and the media with one simple answer…take more calcium. But if you are one of the types that requires other nutrients ahead of calcium, you can end up inadvertently contributing to bone loss in your body.
How homocysteine fits into the discussion
Homocysteine is an amino acid metabolite in the body, produced from the breakdown of proteins. Interaction with B vitamins allows homocysteine to be maintained at healthy levels in the body.
When it interacts with the B vitamins, homocysteine converts to two crucial substances:
Methionine, an essential amino acid and antioxidant that synthesizes (creates) proteins.
Cysteine, a nonessential amino acid synthesized from methionine that reduces inflammation, increases communication between immune cells and increases liver health
Either low levels of B vitamins in the body or a failure of the cystathione beta synthase (CBS) detox pathway can lead to elevated levels of homocysteine. These are both increasingly common occurrences given the exponential growth in toxin levels in our world and the burdens those place on the body. Genetic mutations such as one in the CBS pathway are with us from birth. But they are not always “switched on” - that switch is typically flipped through epigenetic stresses. And once the CBS pathway is compromised, we often see the same in the MTHFR pathway. While this is a huge subject in and of itself, our focus here is on the accumulation of homocysteine and how it impacts bone health and associated mortality rates.
When homocysteine is not broken down effectively into methionine and cysteine, its levels rise in the bloodstream. As this happens, reactive oxygen species (ROS) are created. ROS then activate something called matrix metalloproteinases (MMPs). MMPs have important functions in the body, including apoptosis (death) of cells and chemokine/cytokine inactivation (which assist in immune response). In excess, MMPs will cause excess apoptosis and excess inactivation of important immune responses. They also create bone matrix degradation via excess stimulation of the osteoclasts that control degradation/resorption of bone. In essence, bone formation is quieted and resorption is dominant.
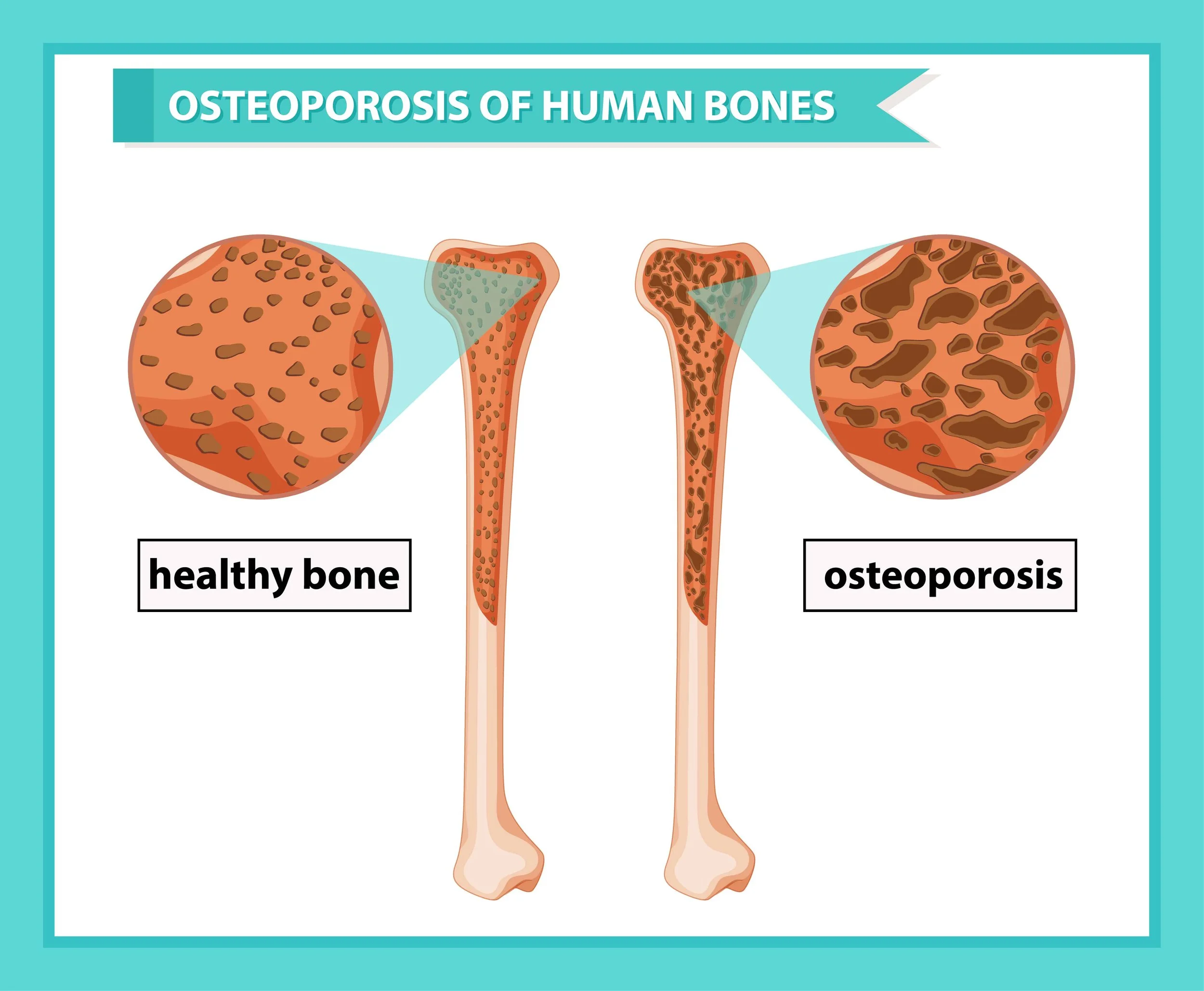
Healthy vs. osteoporotic bone
Returning to the conversation on collagen and bone mineralization, up to 65% of homocysteine can end up binding to the collagen matrix, decreasing mineralization and promoting degradation.
Other critical considerations around homocysteine include its very negative impacts upon the brain/nervous system and the cardiovascular system.
The brain has a limited capacity for homocysteine metabolism. Its presence in excess contributes to issues with neurotransmission as well as neurological diseases such as Parkinsons and Alzheimers. Again, B vitamins are key to homocysteine metabolism. The level of 5 tetrahydrofolate (folate) in the cerebrospinal fluid is 3 times that of the plasma level and there exists an active process to maintain it. Folate deficiency is a common problem.
Equally important - and the #1 cause of mortality with people with bone loss/fractures - is the impact of elevated homocysteine upon the cardiovascular system. People with cardiovascular disease are anywhere from 2 to 4 times more likely to die following a bone fracture than those without bone loss/osteoporosis. Homocysteine is implicated as an early atherosclerotic (plaque) promoter. Fasting serum homocysteine levels in CAD (coronary artery disease) patients are significantly higher than patients without coronary artery disease. Also, homocysteine levels correlate significantly with increasing severity of coronary artery disease. According to this paper, the most common and plausible mechanism for increased risk of CAD are endothelial dysfunction thought to occur primarily from changes in vascular endothelial compliance and platelet coagulation changes that promote cardiovascular disease. This brings us to an important point that I have covered in the past, and those are the contributing mechanisms of nitric oxide and glycocalyx health in endothelial and cardiovascular health. Nitric oxide is also a contributing mechanism with MMPs (discussed above).
Regular testing of homocysteine is part of my practice and is an important consideration in both your detox and cardiovascular profiles.
Are we safe just relying on the medications for osteoporosis?
It appears we are not, and many are calling for a new conversation in the diagnosis and treatment of osteopenia and osteoporosis. Bisphosphonate drugs such as Fosamax stop the development of osteoclasts, specialized bone cells that break down bone as part of the remodeling process (which we discussed earlier). This can create higher bone density, but it also stops remodeling and does not create better bone quality.
Let’s take a look at everything that contributes to overall bone strength (i.e. quality).
Components of bone strength
When you see the myriad of factors that have to be considered around bone strength and remodeling, it is clear that a simple shutdown of one aspect does not solve this complex problem.
Bone strength = QUANTITY + QUALITY
〰️
Bone strength = QUANTITY + QUALITY 〰️
Research has also shown that higher “bone density” without overall quality is associated with higher risk of breast cancer.
Clinical case reports and observations have also indicated that spontaneous large bone (femur) fractures are occurring alongside long-term use of drugs like Fosamax. Insufficient investigations and responses from the drug maker are unfortunately occurring simultaneously.
Two new and supportive bone measurements in the medical world, TBS and REMS
Our first new and very helpful assessment in the process of measuring bone integrity. It is the trabecular bone score (TBS). While the traditional bone scan (DEXA) measures the density of bone, delivering a T score of normal or negative, the TBS measures the quality of bone. Its addition to the assessment equation can make a significant difference in the overall T score. Think of a structure that has only vertical slats to hold itself vs. one that has both horizontal and vertical slats - the integrity/strength of the structure is greater with the latter. The TBS also refers to some degree to the elasticity of the bone. So, those with a negative DEXA T score may be brought to normal by a high TBS. This can mean the difference of prescription of medication or not. And, while we won’t cover that topic here, bone density medications are not considered effective by many practitioners. They can create false increases in BMD that disappear as soon as the medication is removed. Many people with high TBS (which equates to high quality/elasticity) do not break bones in spite of T scores that reveal osteoporosis.
How a high TBS impacts bone integrity
TBS is a software that is added to the clinic’s scanning machine. If you would like to search your area for a clinic offering TBS along with the DEXA scan, visit this site: www.medimapsgroup.com/find-a-clinic-with-tibs/ (You may also consider providing this information to your primary MD and/or DEXA clinic to request addition of the TBS program to their equipment.)
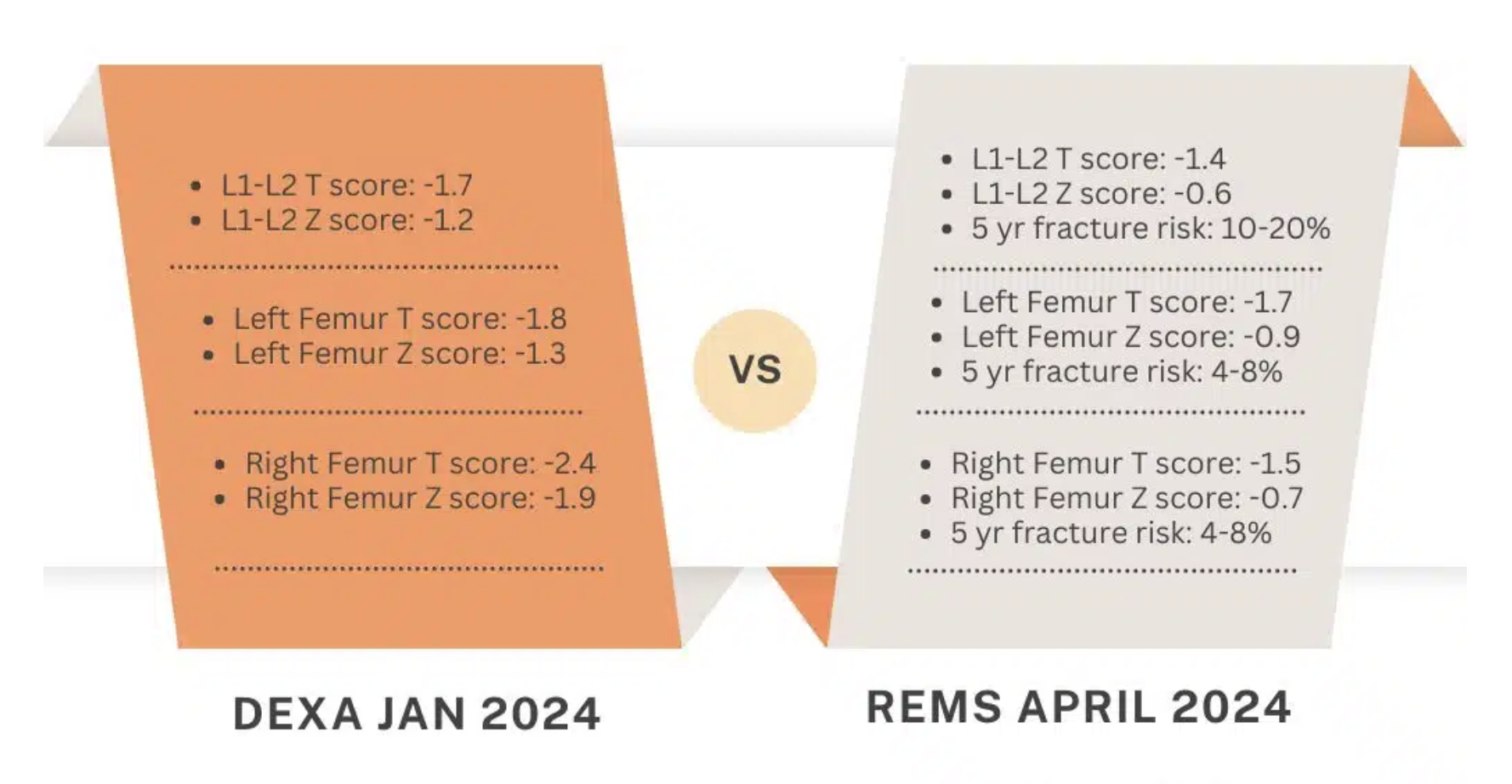
The 2nd new technology that gives us more refined and complete information about bone health is RMS (radio frequency ecographic multi spectrometry). This is the newest “kid on the block”, utilized in Europe for some time and now making its way into the US for practice. A study of over 4,000 female patients with osteoporosis and fracture risk concluded that RMS is equally or more specific and effective at predicting risks than DXA. RMS is conducted with ultrasound, thus making it safer than the radiation of DXA. It also includes multiple assessments which are part of bone integrity/quality vs. DXA which only provides mineral density. As we’ve discussed above, quality matters, inclusive of lean muscle mass connected to bone. Here is an excellent presentation on RMS: https://www.youtube.com/watch?v=6YYInYBKcRQ. You may find centers providing RMS screening by sending an email here: https://www.echolightmedical.com/en/usa-office/
Here is one person’s comparison of DXA & RMS scan scores (note how much better the RMS scores are, due to inclusion of the variety of quality scores:
Comparison of DXA and RMS T scores
The unfortunate new research on microplastics and bone loss
Another factor we must now be concerned with involving bone loss and osteoporosis are the accumulation of microplastics in our environment that have been found in bone tissue and bone marrow.
Researcher Rodrigo Bueno de Oliverira, coordinator of the Laboratory for Mineral and Bone Studies in Nephrology, State University of Campinas in Brazil states: "The potential impact of microplastics on bones is the subject of scientific studies and isn't negligible. For example, in vitro studies with bone tissue cells have shown that microplastics impair cell viability, accelerate cell aging, and alter cell differentiation, in addition to promoting inflammation."
In this comprehensive study review completed by Oliveira and colleagues, there is mention of the negative impacts upon trabecular integrity in the bones:
“Additionally, MPs accumulation in bones reduced their growth and impaired trabecular microarchitecture likely due to the osteoblasts' decreased osteogenic function.”
As we have previously discussed here, the consideration of tensile strength in trabecular structure inside of the bone (vs. outer layer) is crucial as it relates to bone fragility. If microplastics are breaking down the inner layers by stimulating too many osteoclasts, no drug that is designed for outer layer thickening will help. Fragility risk and bone fracture rates will rise significantly. And along with fracture rate increases go increases in mortality rates.
The promise of PEMF treatment for bone regeneration
Another promising option for those dealing with bone loss is that of PEMF (pulsed electromagnetic field) therapy. In the most recent review (2025) of studies related to bone growth stimulation via PEMF, both overall bone growth and repair of bone fractures were shown to be positively impacted.
Specialized PEMF mats and control units allow at-home freedom for daily treatments. Please contact me for more details on this matter.
Here, see the summation of bone and cartilage responses to PEMF:
PEMF, bone & cartilage tissue improvements
Summations and Solutions
Osteopenia and osteoporosis are health concerns for both men and women. Alongside the presence of bone loss come concerns for proper nutrition, proper detoxification and homocysteine control, and proper diagnostic methods.
It is advised to consider all of the following as you track your bone health over the years:
Personalized nutrition needs, including mineral intake - both doctors and media-based practitioners can make broad-stroke supplement recommendations that can be detrimental to liver health. Know what your body needs.
Evaluate thyroid and parathyroid health through blood testing, as well as homocysteine (See list of risk factors here)
Exercise, especially weight-bearing, and particularly for those diagnosed with osteopenia or osteoporosis, force-loaded (bone end-to-end force) exercise. Forms of osteogenic force-loading exercises may be reviewed here. (Always consult with your doctor and/or a professionally trained physical therapist before initiating specialized training programs.)
Vascular, gut and immune health
Avoid excess sugar, alcohol, caffeine and wheat, which are known to decrease bone integrity
Use of appropriate diagnostic scans, including DEXA, TBS and/or REMS, considering you may be better off to pay out of pocket for diagnostics and treatments that will spare the potential deductibles/added costs and associated mortality risks that come with osteoporosis
Use of PEMF therapy
Consider a grounding sheet for your bed. While research is lacking, there is considerable empirical evidence that grounding supports bone health.
Use of CBD for bone strength and mass
Use of shilajit for osteoblast stimulation
Daily use of collagen peptides has been researched to improve bone health, as has the inclusion of daily use of orthosilicicic acid (OSA)
Osteoporosis and collagen peptide consumption
Bone health and orthosilicic acid
Contact me today at Julie@truenaturehealthconsulting.com to investigate your personal risks and whole health needs. True Nature Health Consulting provides holistic telehealth services.
Originally published March 2022
Updated February 2025
This information is provided for educational purposes and is not intended to treat or cure disease.