Cholesterol and the Big Fat Myths
Hello, I am Julie Donaldson and I am a clinical nutritionist with functional health training. I specialize in restoring balance in complex, chronic and acute health conditions. I welcome you to peruse other articles that may be of interest to you in your health investigation!
“I had always been told that since there was family history of “high” cholesterol, I would need to take medication for the rest of my life. No one ever discussed other issues that also ran in my family and our genetics, nor how to functionally manage those issues. Julie is this person. Not only am I off medication but all those other issues are successfully addressed and I am healthier than ever. She is simply amazing.”
If there was ever a “big fat” myth, it’s that of low cholesterol being “good” for us. Like most health care myths, there is a lot to break down on this subject and it is never a black and white scenario. But when clients are constantly having anxiety about their cholesterol levels because of conventional ideas…it’s time to have this conversation. I have it one-on-one multiple times weekly, but now we’re going to lay out some evidence-based research on cholesterol and where we truly need to land with our personal investigations. It’s a hefty topic, but fear not, I’m going to break it down for you and summarize the solutions.
Is there really a connection between saturated dietary fat, cholesterol and heart disease?
No. This compilation of research data over 18 years and tens of thousands of patients states very plainly: “A meta-analysis of prospective epidemiologic studies showed that there is no significant evidence for concluding that dietary saturated fat is associated with an increased risk of CHD or CVD.” So, why do we continue to hear this false claim being made in the media and medicine communities? Great question. There are occasional singular studies done with some negative indicators resulting…but as I’ve said in the past…we cannot study a population of people being fed unclean, conventional foods whose personalized nutrition needs are widely variable and consider that an answer to the question. Nearly any person who eats unclean food that is contrary to their body’s individual needs will develop system imbalances and disease over time. When do you read a study done over a long period with sustainable, organic food?
Secondly, research is (very wisely) pointing towards the multitude of pathogenic and dietary variables that contribute to higher cholesterol numbers. From this study, researchers state the following:
“Due to the highly variable intake of fatty acids in humans and other omnivore species, we propose that circulating lipoproteins serve as a buffer to enable the rapid redistribution of cholesterol molecules between specific cells and tissues that is necessary with changes in dietary fatty acid supply. Hence, circulating levels of LDL cholesterol may change for nonpathological reasons. Accordingly, an SFA (saturated fatty acid)-induced raise in LDL cholesterol in healthy individuals could represent a normal rather than a pathologic response. These regulatory mechanisms may become disrupted secondarily to pathogenic processes in association with insulin resistance and the presence of other ASCVD (atherosclerotic cardiovascular disease) risk factors, as supported by evidence showing diverging lipoprotein responses in healthy individuals as opposed to those with metabolic disorders such as insulin resistance and obesity. Corresponding with the model, we suggest alternative contributing factors to the association between elevated LDL cholesterol concentrations and ASCVD, involving dietary factors beyond SFAs, such as an increased endotoxin load from diet-gut microbiome interactions and subsequent chronic low-grade inflammation that interferes with fine-tuned signaling pathways.”
We’ve discussed how inflammation = disease. My clients always, always hear that cholesterol will go up in the presence of chronic inflammation. This paper explains that variable conditions with fatty acid intake combined with pathogenic activity, endotoxins (produced by pathogens) and microbiome interactions are inevitable amongst individuals. While the medical model of cholesterol and heart disease is based upon standards and the same types of expression and risk for all people, in the functional world, we absolutely know it to be the truth that we are all biochemical individuals and thus must be evaluated and considered as such.
Related to this conversation about circulating levels of LDL, let’s bring in the topic of taurine and its role with cholesterol. Adequate supplies of taurine in the body contribute to healthy LDL levels, up to 37% lower. (I know you’ve heard it said that LDL is the “bad cholesterol”. There is no such thing…different forms of cholesterol have different tasks, none of which are “bad”. LDL is returning cholesterol molecules to the liver for synthesis. The question we need to be asking is what is unresolved that is preventing cholesterol from being most efficiently synthesized and utilized.)
Taurine is an amino acid, and it is the only sulfated amino acid. It is not one of the “essential” amino acids, but rather what is called a conditionally essential amino acid - this means that it is needed in times of illness and stress vs. as a building block for protein. Taurine makes up 50% of the free amino acid pool in the heart and is found in high levels also in the brain, liver and eyes. Like all amino acids, taurine is found in animal protein. And what often happens when someone is suspected of having heart disease? They are advised to reduce/avoid animal proteins due to the “saturated fat” myth. Talk about some diet dogma…again, clean animal protein is a must, but avoidance can mean giving credence to the wrong theory of the root of the disease.
And here is another connection with taurine and the variable factors outlined above: healthy bacteria in the gut are needed to synthesize taurine into sulfate. This finds us circling back to the understanding that fatty acids and gut bacteria (which interact with each other) are playing a role in the production of cholesterol sulfate and the modulation of stored lipid-based cholesterol molecules.
A truly fascinating fact about taurine is that, in cardiac emergency, a heart attack can initiate a programmed response that unloads taurine reserves to restore sulfate supplies. Stephanie Seneff, PhD writes as follows:
“Human white blood cells produce an enzyme called myeloperoxidase (MPO) during ischemia and reperfusion injury. Elevated MPO is an established risk factor for cardiovascular mortality following artery grafts. MPO often serves as a potent bacteriocidal weapon, potentially linking it to the infectious theory of heart disease. Hypochlorite, produced in response to MPO, avidly oxidizes many sulfhydryl-dependent proteins, leading to platelet activation and causing white blood cells to attach to the walls of blood vessels. It has been proposed that taurine protects from these damaging effects by reacting with and neutralizing hypochlorite to form taurine chloramine, a much more reactive compound than taurine. As we have seen, taurine is released from the heart during ischemia and would be readily available in the serum because it is not taken up by the platelets.”
Let’s dive into a much more relevant view of where the risks are likely occurring.
Cholesterol sulfate and the protection of blood vessels, endocalyx and blood flow
There is a plethora of information about the protection of our blood vessels, red blood cells and endocalyx that comes from the production of cholesterol sulfate. Red blood cells, platelets and cells in the skin synthesize cholesterol sulfate catalyzed by sunlight. Cholesterol sulfate, unlike cholesterol (fat soluble), is water soluble, so it can travel freely in the blood vs. being packaged inside an LDL particle. Sulfate provides a negative charge in the blood vessel wall and maintains the structured water that lines the vessel walls with a slick, frictionless surface.
What we know about cardiovascular disease and cholesterol is that there is an accumulation of the lipid particles in the arteries (not the veins) supplying the heart. These accumulations produce arterial plaque…but they are accumulations of pure cholesterol molecules waiting to be synthesized into cholesterol sulfate. Cholesterol gets stored in the artery wall to be made readily available for cholesterol sulfate synthesis whenever precursor sulfur sources such as (homocysteine or cysteinylglycine) are available. ATP, oxygen and superoxide provide the energy to fuel the synthesis. The absolutely critical first step, however, is the stimulation of synthesis via sunlight exposure on cholesterol molecules in the skin. Normally, keratinocytes in the skin, red blood cells (RBCs) and platelets produce cholesterol sulfate from precursors, catalyzed by sunlight. Low sun exposure is associated with higher rates of heart disease. Indeed, geographical data show an inverse relationship between cardiovascular disease and annual sunlight availability. France and Spain have much lower rates of death from heart attacks than the United Kingdom. In a study conducted in the British Isles, mean annual sunshine hours accounted for 49 percent of the variance in mortality from coronary heart disease. Interestingly, however, as we typically move straight to the idea of vitamin D supplementation in the presence of low sun exposure, such supplementation does not change the risk of heart disease…supplementation with sulfur-rich foods does. (Here you may find more information on the effective processing of vitamin D via sun exposure.)
Adequate nitric oxide production plays a major role here as well. I have written about nitric oxide in relationship to cardiovascular disease, diabetes and immune function as well as gut health. Once again, here we find ourselves in the territory of intersecting body systems and the ramifications for overall holistic health. No system in the body exists in a vacuum by itself - everything is intersecting and interdependent.
This conversation cannot be complete without discussing the glycocalyx. The glycocalyx is a complex mesh of sulfated sugar chains lining the interior wall of all blood vessels. It is paramount to vascular health. Heparan sulfate proteoglycans (HSPGs) in the glycocalyx play many important roles, mediating cellular signaling mechanisms and promoting uptake of various nutrients. Clearance of LDL cholesterol particles by liver cells is promoted by the HSPGs in the glycocalyx as well.
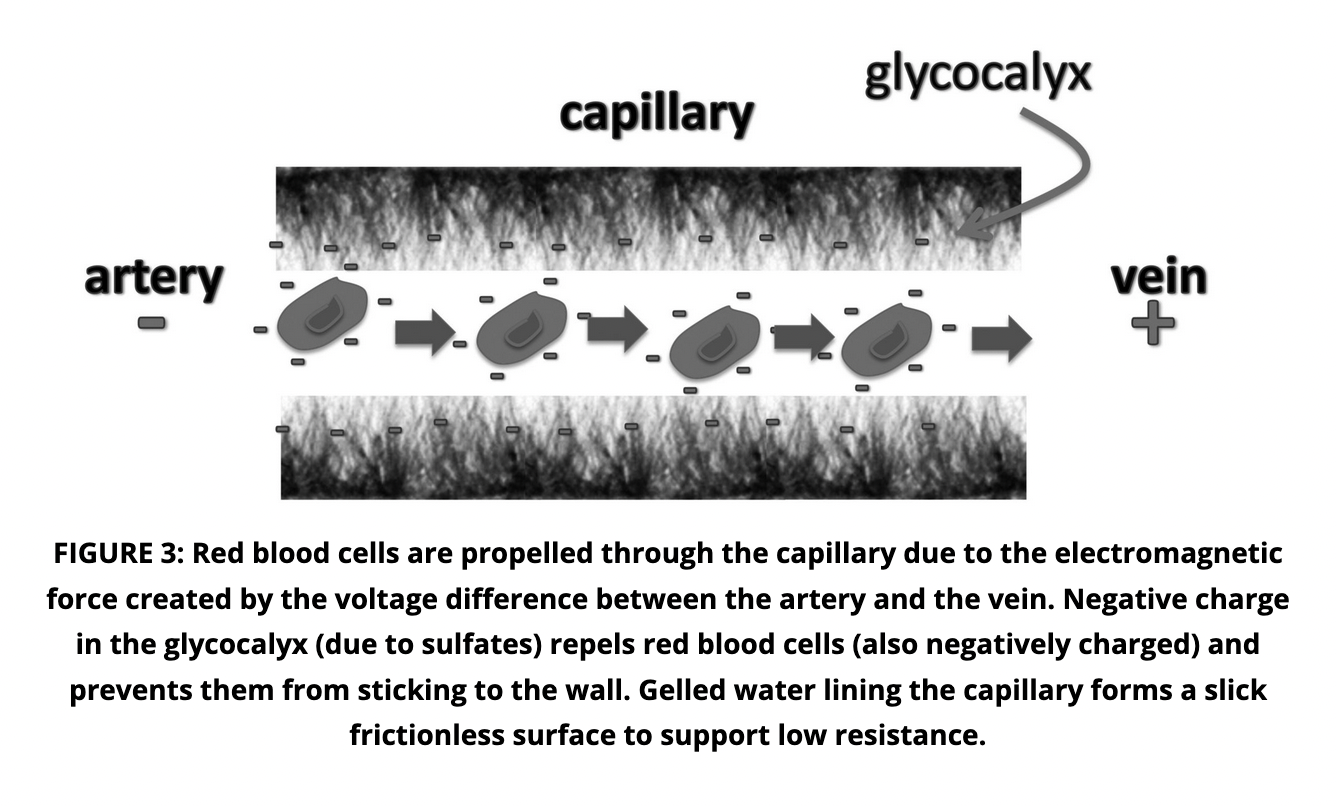
Glycocalyx, artery, vein, capillary flow
Once cholesterol sulfate is provided in the blood stream and heart, it is fed into the capillaries. The most important role of cholesterol sulfate in the capillaries is to maintain a thick layer of gelled water coating the inner surface, the glycocalyx. This structuring effect on water is due to the “kosmotropic” properties of sulfate, which provides a near-frictionless surface contact with the red blood cells that is further enhanced by the negative charge in both the glycocalyx and the red blood cell membrane. It is this frictionless surface that prevents the buildup of molecules that can produce plaque.
Low cholesterol, optimal cholesterol, statins and mortality rates
Inflammation damages the lining of your arteries. It actually causes wear and tear to the once-smooth inner lining of artery walls. Once lesions develop in the arteries, the body sends cholesterol in an attempt to repair the damage. Cholesterol is your body’s #1 steroidal hormone. It is the primary molecule providing the base of corticosteroid hormones produced in the adrenal glands, whose job it is to reduce inflammation. Without them, we would just inflame our lives away, as the corticosteroids mitigate inflammation from all kinds of pathogens, including bacteria, viruses, fungi, molds, etc. They also support recovery from inflammatory processes/wear and tear in the muscles, tendons, ligaments and bones. Simply because cholesterol is present when arterial plaque is formed does not mean it caused the plaque. Inflammation from any number of potential issues is what initiated plaque formation. This misconception is responsible for many theories of low cholesterol being “healthy” for us.
Low cholesterol and/or poor cholesterol balance is associated with neurodegenerative diseases and neuropsychiatric disorders. The brain and nervous system are 60% fat - dehydration from fat can occur in the body as much as it can with water. Cholesterol is the main component of the cell membrane; it controls permeability and rigidity of the cellular membrane, aiding in what moves into and out of your body’s cells and regulating membrane homeostasis.
In one of the largest-ever studies of nearly 13,000,000 adults over a period of 10 years, it was determined that the total cholesterol (TC) range associated with the lowest mortality was 210–249 mg/dL. When age was further considered, U-curve associations were observed regardless of sex or age, and the optimal TC range for survival remained at 210–249 mg/dL. This is in contrast with current “optimal” medical ranges for cholesterol between 100-199 mg/dL. In this study, in a TC range of 50-199 mg/dL, for every increase of 39 mg/dL, there was a 23% decrease in mortality rate.
Study authors state:
“Hemorrhagic stroke, respiratory diseases (especially chronic obstructive pulmonary disease), digestive diseases (especially liver disease), and several cancers have been suggested to be associated with lower TC levels; thus, the ranges associated with lowest risk might be even higher for these diseases than those for all-cause mortality. However, we could not examine whether the associations differed by cause of death, due to data unavailability.”
In another study completed by researchers at Harvard and MIT, optimal TC was defined at 250 mg/dL. Again, these findings absolutely go against the grain of conventional ideas of low cholesterol being helpful and healthy.
The one conflicting area exists where those with many complicating diseases (such as diabetes & metabolic syndrome) are studied. Mortality rates in high disease states climb with higher TC. This may very well link us right back to earlier discussions of damaged artery walls & glycocalyx and thus impaired sulfation and immune responses. Once a systems-wide inflammatory and disease process has set up, management of such is often required on different terms from that of a healthier body.
This population calls up the question of statin use/efficacy and the broad-stroke recommendation for anyone with elevated cholesterol to utilize statins. Research, however, shows that statin use can produce the disease it is intended to “cure”. In this 2015 paper, authors state the following:
“In contrast to the current belief that cholesterol reduction with statins decreases atherosclerosis, we present a perspective that statins may be causative in coronary artery calcification and can function as mitochondrial toxins that impair muscle function in the heart and blood vessels through the depletion of coenzyme Q10 and 'heme A', and thereby ATP generation. Statins inhibit the synthesis of vitamin K2, the cofactor for matrix Gla-protein activation, which in turn protects arteries from calcification. Statins inhibit the biosynthesis of selenium containing proteins, one of which is glutathione peroxidase serving to suppress peroxidative stress. An impairment of selenoprotein biosynthesis may be a factor in congestive heart failure, reminiscent of the dilated cardiomyopathies seen with selenium deficiency. Thus, the epidemic of heart failure and atherosclerosis that plagues the modern world may paradoxically be aggravated by the pervasive use of statin drugs. We propose that current statin treatment guidelines be critically reevaluated.”
More direct prediction of cardiovascular disease via triglyceride levels
Triglycerides are an important cholesterol in your body. They constitute the main source of energy for the body. Exogenous triglycerides originate from food, while endogenous triglycerides are formed in the liver. Once digested, triglycerides from fats and nutrients become the main energy reserves for the body, stored in the muscles. They take part in metabolic processes that determine the rate of fatty acid oxidation, the plasma levels of free fatty acids, the biosynthesis of other lipid molecules and the metabolic fate of lipoproteins. Muscle maintenance and activation are key elements in the use of these energy reserves.
An adequate supply of triglycerides (functionally, ranging between 50 and 100) is necessary to fuel the body. On the other hand, excesses are the most risky of all high cholesterol markers in connection with cardiovascular disease.
There are decades of research and direct correlation of elevated triglyceride levels and heart disease. The National Health and Nutrition Examination Survey has tracked increasing mean triglyceride levels for more than 30 years. One third of the U.S. population has at least borderline elevated triglycerides. Over 16% of the U.S. population has high to very high triglyceride levels. The trend amongst younger people in the U.S. is the most disturbing in that its upward motion is persistent. This trend runs alongside increasing obesity, insulin resistance and diabetes and metabolic syndrome since 1976. These co-conditions are proven to accompany triglycerides in creating higher risk for disease.
Triglycerides serve as the best direct predictor of cardiovascular disease, compared to those of LDL and HDL. Triglyceride rich lipoproteins (TRLs) create smaller, denser LDL and HDL particles in the bloodstream that are dysfunctional and more susceptible to oxidative stress. These factors contribute to atherosclerosis. Foam cell formation also accelerates senescence (loss of innate function) and interfere with endothelial blood vessel wall repair - we discussed this earlier in the article. Foam cells are a type of macrophage that localize to fatty deposits on blood vessel walls, where they ingest low-density lipoproteins and become laden with lipids, giving them a foamy appearance.
In the above-reference research, there is also important information about the preference for utilizing non-fasting triglyceride testing where there is suspicion of possible disease. In a non-fasting test, a postprandial (post-meal, glucose elevation) state enriched in dietary fat may affect saturation parameters and impede the liver’s removal of circulating CMRs (chylomicron remnants, which carry lipoprotein molecules), thereby permitting their uptake and incorporation by macrophages. Studies have recently identified nonfasting triglyceride levels to be a superior predictor of CVD risk compared with fasting levels which have historically been the testing standard.
What causes elevated triglycerides? There can be many causes, but the most common are:
Poor diet, inclusive of excess nutrient intake - most commonly simple carbohydrates and sugars, but can be any nutrient excess
Consistent and/or excessive alcohol consumption
Genetic mutations (especially in childhood cases)
Poor kidney function and/or disease
Cholesterol and methylation
We would be remiss in failing to make mention of the very important connection between balanced methylation and cholesterol metabolism. Again, assessment of and discussions on methylation function are common-course here at True Nature. The body’s ability to maintain and utilize methyl donors in the process of detoxification is key to health. Methyl donors are required in order to break a toxic substance down into a water soluble form that can be excreted from the body via the bowels and kidneys/bladder. The methyl group can directly be delivered by dietary methyl donors, including methionine, folate, betaine, and choline. The liver and the muscles are the major organs for methyl group metabolism. A large percentage of the population has has expressions of either over or under-methylation. Either of these patterns can lead to failed DNA methylation with cellular damage resulting.
Many people have received genetic testing and will say “I have MTHFR”…it’s a bit of a catch-phrase and has populated functional health discussions for some years now. But what does this mean? Honestly, it means nothing unless the gene mutation switch is “flipped on”. Most of us have multiple gene mutations but may not be suffering functional expressions of them. It is imperative to investigate bio-chemically in order to understand what is actually expressing.
In this paper, the disease risks associated with over or under-methylation and co-factor deficiencies, cholesterol levels and cardiovascular disease are addressed. Metabolism of folate, betaine, choline, and methionine are interrelated and key to normal, balanced methylation function. Deficiency of dietary methyl donors can cause metabolic and functional disturbances. Metabolic changes in the cell are reflected by elevated homocysteine levels, disturbed energy and lipid metabolism, and dysregulation of DNA methylation and protein synthesis. (Note: many doctors understand the value of testing homocysteine in relationship to CVD risk. Few, however, understand the value of its connection with methylation.)
Choline-rich food sources include:
grains
meat
eggs
Betaine-rich food sources include:
beets
spinach
grains
Methionine-rich food sources include:
meat
eggs
dairy
beans
So, as you can see once again, typical “low cholesterol” nutritional recommendations can exclude many of the foods necessary to support both methylation and amino acid synthesis. Meat, eggs, dairy and beans are all foods with high sulfur content that can support cholesterol sulfation.
Summations and solutions
First, here is a summary of the article’s key points:
Saturated fat consumption is not scientifically correlated with cardiovascular disease
Elevated triglycerides are the most direct predictor of cardiovascular disease.
Cholesterol sulfation is the key to utilizing cholesterol molecules most efficiently in the body. Sufficient sulfur foods and substances are necessary for this to occur, as is direct sunlight exposure on the skin.
Meat, eggs, dairy, grains, beans, MTcruciferous and onion family foods are the main sources of dietary sulfates.
Taurine is an amino acid required for cardiovascular health. 50% of the free amino acid pool is in the heart. Taurine is partially synthesized into sulfate by healthy bacteria in the gut.
Research shows that pathogens and immune inflammation are a major cause of endothelial blood vessel and glycocalyx damage/destruction, both of which are connected to cardiovascular disease.
Statins are known to contribute to atherosclerosis via Co-Q 10, heme and ATP depletion as well as the blocking of vitamin K. These conditions encourage calcification in the blood vessels.
Higher total cholesterol correlates with lower mortality rates.
Cholesterol synthesis is also dependent upon successful methylation and the presence of methyl donors such as choline, methionine and betaine.
It’s time to talk about what to do…
Eat by your personal MT®. In this article, you see multiple references to ATP. ATP is produced as a result of successful mitochondrial respiration, driven by balance in the Krebs cycle, all of which MT® supports.
Eat organically and ecologically to the largest extent possible. Another connection with cholesterol and sulfation is the negative presence of glyphosate in nearly all conventional food sources. Glyphosate disrupts CYP enzyme activity in the liver, which can explain the contribution of glyphosate to hyperlipidemia. Multiple CYP enzymes are needed to produce bile acids, which facilitate digestion and absorption of lipids and regulate cholesterol homeostasis. Bile acids normally export a large amount of cholesterol via the digestive system. Impeded bile acid synthesis due to a defective CYP7A1 gene is switched on by epigenetic factors. This produces blocked bile ducts.
Maintain individually-appropriate consumption of meats, eggs, dairy, grains, beans and sulfur-rich vegetables such as those in the onion and cruciferous families.
Utilize appropriate therapeutic protocols with sulfur-rich supplements such as NAC, glutathione, glucosamine sulfate, chondroitin sulfate and MSM.
Consider the power-duo of bergamot and artichoke while you investigate and get to the roots of your high cholesterol. The combination of these two powerful compounds are effective not only on lipid metabolism, but also on oxidative stress and vascular inflammation. Bergamot contains potent polyphenols while artichoke is highly cholagogic (referring back to the bile acid/ducts conversation).
Complete your annual physical with your MD, assessing all familial and personal risk factors, blood pressure, heart rate and overall health.
Test immune, metabolic, lipid and methylation function at least twice annually. More frequent follow-up may be appropriate when imbalances have been located. These results should be supervised by a highly trained and experienced functional health practitioner.
Please reach out to me at Julie@truenaturehealthconsulting.com if I may assist your personalized investigation. We provide holistic telehealth services.